Signs of a Heart Attack Everyone Should Know
Signs of a Heart Attack
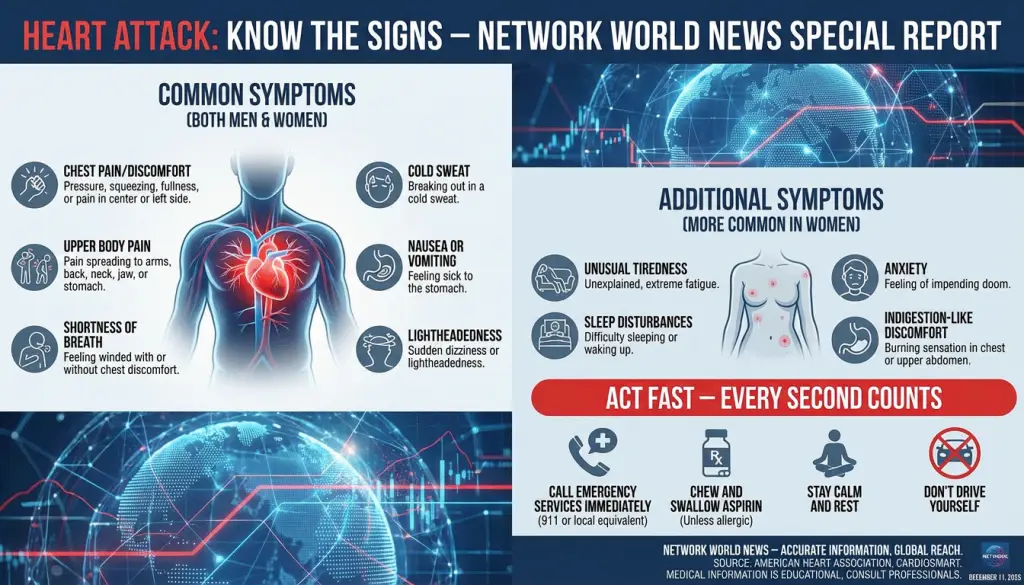
Signs of a Heart Attack. Every minute is critical when heart attack symptoms appear. A heart attack occurs when blood flow to the heart is blocked. This blockage is usually caused by plaque in the coronary arteries. Significant Warning Signs of a Heart Attack (Most Common)
1. Chest Pain or Discomfort
- Classic symptom: pressure, squeezing, fullness, tightness, or a “heavy weight” on the chest
- Can feel like:
- Burning
- Cramping
- Sharp pain (less common, but possible)
- “Elephant on the chest” sensation
- Duration: usually > 5 minutes; may come and go
- Often NOT relieved by rest
2. Pain Radiating to Other Areas
Pain may spread to:
- Left arm or both arms
- Neck
- Jaw
- Back (especially upper back between shoulder blades)
- Shoulders
- Upper stomach area (can be mistaken for indigestion)
This pain may be dull, pressure-like, or achy—not always sharp.
3. Shortness of Breath
- Difficulty catching breath
- Feeling winded at rest
- Sudden breathlessness without chest pain (widespread in women)
- May feel like you “can’t get enough air.”
4. Nausea, Vomiting, or Indigestion
- Often mistaken for food poisoning or acid reflux
- May accompany chest pressure or occur alone
- More common in women
5. Cold Sweat
- Sudden sweating unrelated to heat or activity
- Skin may feel clammy or pale
- Often described as a “stress sweat.”
6. Lightheadedness or Dizziness
- Feeling faint or like you might pass out
- Can occur with or without chest discomfort
7. Extreme Fatigue
Women may experience this for hours or days before a heart attack
Sudden unusual tiredness
Feeling “drained,” weak, or unable to continue regular activity
The Mayo Clinic explains that when a plaque ruptures, a clot forms. This clot cuts off the oxygen supply, quickly damaging the heart muscle. See our other top Health reports.
Common signs of a heart attack include chest pain or pressure. This pain can feel like tightness, squeezing, or aching. It may also spread to the shoulders, arms, back, neck, jaw, teeth, or upper belly.
Other symptoms include shortness of breath, cold sweat, nausea, fatigue, lightheadedness, or heartburn-like discomfort. These can also be signs of a heart attack.
Not everyone experiences the same heart attack symptoms. Some feel severe pain, while others notice mild or vague symptoms. Women might have different signs, such as brief or sharp neck, arm, or back pain, or shortness of breath without chest pain.
If you’re unsure, call 911 right away. Recognizing heart attack signs early and acting quickly can save lives.
Signs of a Heart Attack Key Takeaways
- Chest pain or pressure plus spreading discomfort can signal a heart attack.
- Shortness of breath, cold sweat, nausea, or lightheadedness are key signs of a heart attack.
- Women may have atypical heart attack warning signs without classic chest pain.
- Symptoms can start suddenly or build over hours, days, or weeks.
- At the first sign of a heart attack, call 911—immediate care protects the heart muscle.
- If angina does not ease with rest or medicine, treat it as an emergency.
What a Heart Attack Is and Why Time Matters
A heart attack occurs when blood flow to part of the heart stops. Without oxygen, heart muscle cells die. This is called a myocardial infarction, a serious condition.
Time is critical because the heart muscle is fragile without oxygen. Quick treatment leads to better results. It means fewer heart rhythm problems and a shorter recovery time.
How blocked coronary arteries trigger a myocardial infarction
Coronary arteries carry oxygen-rich blood to the heart. If one gets blocked, the heart muscle starves. A complete blockage causes fast damage, while a partial blockage can also harm tissue.
Doctors use door-to-balloon time to measure urgency. Early treatment helps restore blood flow and reduces scarring. Staying healthy and keeping the mind sharp with Keytones. See Keytone report.
Plaque buildup, rupture, and clot formation explained
Atherosclerosis is the leading cause of heart attacks. Over time, plaque builds up in artery walls, narrowing them. If the plaque ruptures, it exposes its contents, which trigger a clot.
This clot can block blood flow, leading to a myocardial infarction. Knowing about atherosclerosis and watching for warning signs can help you act quickly. For more information, see this resource on heart attack and treatment timing.
Why calling 911 immediately saves the heart muscle.
Calling 911 starts rapid care. Emergency services provide oxygen, check heart rhythm, and alert the hospital team. This shortens the time to receive clot-busting drugs or to undergo a procedure to open the artery.
It’s best not to drive yourself. In the United States, calling 911 is the fastest way to get expert help. It’s key to recognize heart attack warning signs when suspected atherosclerosis is present.
Core Heart Attack Symptoms to Recognize Quickly
It’s essential to know the early signs of a heart attack. This way, you can react quickly. Heart attack symptoms can start suddenly or slowly over time. Some people feel severe pain, while others notice only mild discomfort.
Chest pain or pressure: tightness, squeezing, or aching
Chest pain is often described as pressure or tightness. It can feel like a band around your chest. If it lasts more than a few minutes, don’t wait to see if it goes away.
Pain radiating to arms, back, neck, jaw, or upper belly
Pain can spread to your arms, back, neck, jaw, teeth, or upper belly. This can happen with or without chest pain. If you feel pain spreading, it’s a sign to act fast.
Shortness of breath, cold sweat, nausea, lightheadedness
Shortness of breath can happen with or without chest pain. You might also feel cold sweat, nausea, or get dizzy. These symptoms together are strong signs of a heart attack and need immediate action.
When in doubt, treat new, intense, or unusual symptoms as urgent. A fast response can make a critical difference.
Signs of a Heart Attack
Less Common but Serious Signs
8. Anxiety or a Sense of Doom
-
Strong feeling that something is very wrong
-
Sudden panic-like symptoms without cause
9. Upper Abdominal Pressure
-
Can feel like severe heartburn
-
Pressure may worsen when bending forward or lying down
-
Pain may radiate to the back
10. Irregular or Rapid Heartbeat
-
Palpitations
-
Feeling like your heart is skipping beats
-
Heart racing without exertion
-
Not always a heart attack, but it is dangerous if combined with other symptoms
11. Arm Weakness or Numbness
-
Especially in the left arm
-
May be constant or come and go
-
Tingling that climbs up or down the arm
Signs More Common in Women
Women often experience “atypical” symptoms:
-
Shortness of breath without chest pain
-
Sudden unexplained fatigue
-
Jaw pain
-
Back or upper abdominal pain
-
Nausea or vomiting
-
Dizziness
-
Light pressure in the chest instead of sharp pain
Women’s symptoms can be milder and easily dismissed.
Silent Heart Attack Signs (Non-Typical Presentation)
Some heart attacks occur with very mild or non-classic symptoms:
-
Mild chest discomfort mistaken for indigestion
-
Slight shortness of breath
-
Fatigue that feels like you are “coming down with something.”
-
Pressure that goes away quickly
-
Mild discomfort in the back or jaw
-
Symptoms lasting hours to days
Silent heart attacks are more common in:
-
People with diabetes
-
Older adults
-
Women
When to Seek Emergency Help
Call emergency services immediately if:
-
Chest discomfort lasts longer than 5 minutes
-
Symptoms improve and return
-
There is severe shortness of breath
-
Pain radiates to the jaw, arm, or back
-
Someone collapses, becomes unresponsive, or has trouble breathing
Time is critical. The heart muscle begins to die within minutes.
It’s essential to watch for signs of a heart attack, which can be obvious or hidden. Symptoms often start with chest pressure, shortness of breath, and cold sweat. Any new, unexplained chest or upper-body discomfort needs quick attention.
Typical versus atypical presentation across individuals
Typical signs include central chest pain that feels like pressure or squeezing. This pain can move to the arm, jaw, neck, back, or upper belly. People might also feel dizzy, nauseated, or break into a sweat.
Atypical signs are different. They can experience shortness of breath, back or jaw pain, lightheadedness, fatigue, or indigestion without strong chest pain. These symptoms are significant and need urgent care.
Heartburn-like discomfort versus severe chest pain
Not all heart attack signs are crushing. Some feel like heartburn after eating or while resting. Others might feel only mild pressure that comes and goes.
Severe pain is a clear warning sign. But so is a dull, spreading ache that won’t go away. If unsure, check trusted sources on heart attack symptoms to understand different patterns.
When symptoms appear gradually, hours to weeks in advance
Heart attack warning signs can develop over time. Chest pressure with activity that eases with rest may return more often or last longer.
If symptoms change—stronger discomfort, shorter recovery, or new shortness of breath—they signal risk. Treating recurring, stubborn symptoms as a warning to seek medical help is key.
Key reminder: Intensity does not predict danger. Even mild symptoms can mean a blocked artery, so acting quickly is vital.
Women’s Heart Attack Symptoms Can Look Different
Women often notice signs that don’t fit the usual heart attack picture. Knowing these signs helps them get help quickly. This can lead to better heart health. For more on women’s heart attack symptoms, check out the American Heart Association.
Pay attention to brief, shifting pain or discomfort that seems out of place. Many report a sudden stab or a tight pull that fades, then returns. These patterns may be subtle, but they are not normal.
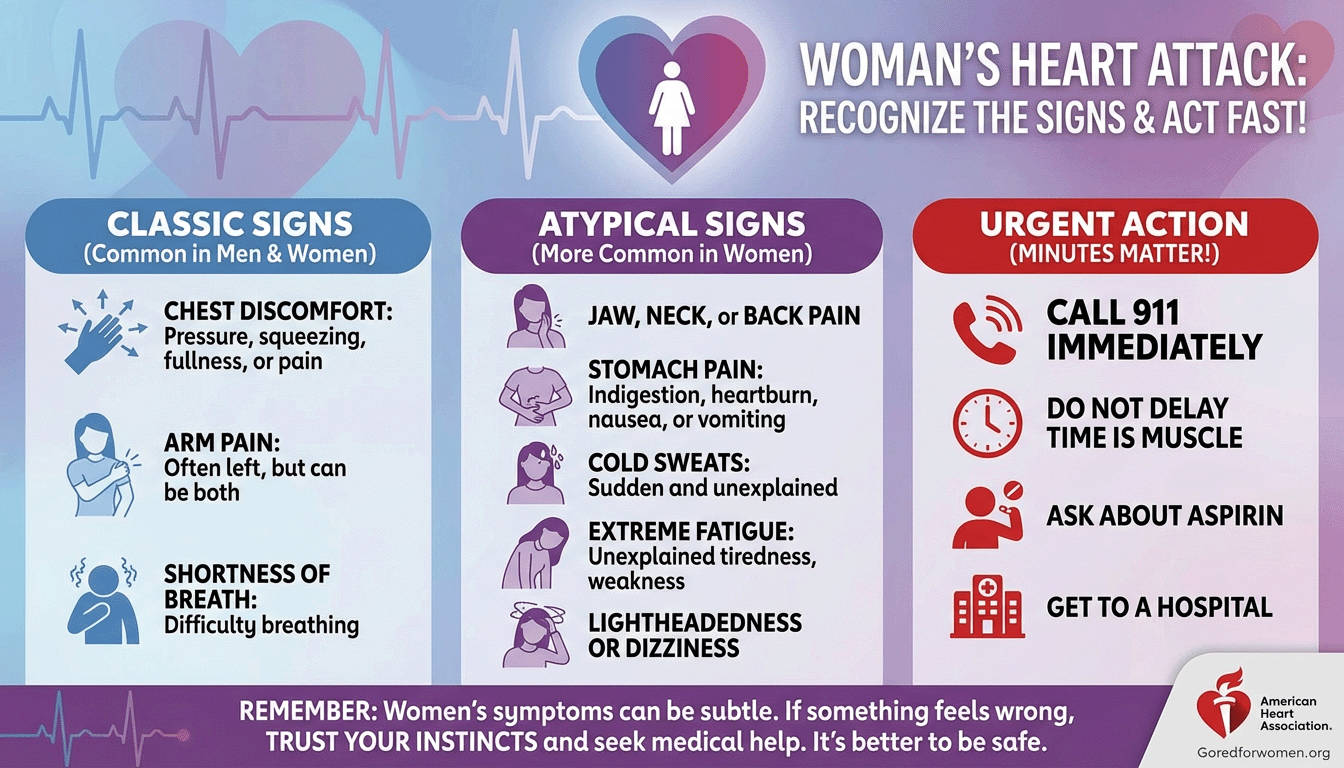
Brief or sharp pain in the neck, arm, or back
She may feel quick, sharp pain in the neck, shoulder, back, or arm. It can strike one side or move around. This may occur without crushing chest pressure, yet it counts as a heart attack symptom.
Some describe a band of pressure across the upper back or a squeeze under the shoulder blade. Tingling in the arm or jaw can follow. Treat these as possible signs of a heart attack in women, not as muscle strain.
Shortness of breath, fatigue, and indigestion without chest pain
Shortness of breath can arise at rest or with light activity. It may be accompanied by nausea, cold sweat, or lightheadedness. Profound fatigue that feels new or unusual is another red flag.
Indigestion, queasiness, or a burning upper belly can appear without chest pain. Because these mimic reflux or the flu, people often dismiss them. Recognizing these patterns supports heart attack prevention and faster care.
Why atypical symptoms delay care and how to respond
When symptoms do not match the “movie heart attack,” many wait to see if they pass. That delay can raise the risk of severe damage. The safest choice is to call 911, rest while waiting, and follow clinical instructions for medicines.
If nitroglycerin was prescribed, use it as directed. Take aspirin only if a clinician or EMS advises it. Acting on these heart attack symptoms right away can protect the heart muscle and align with smart heart attack prevention steps.
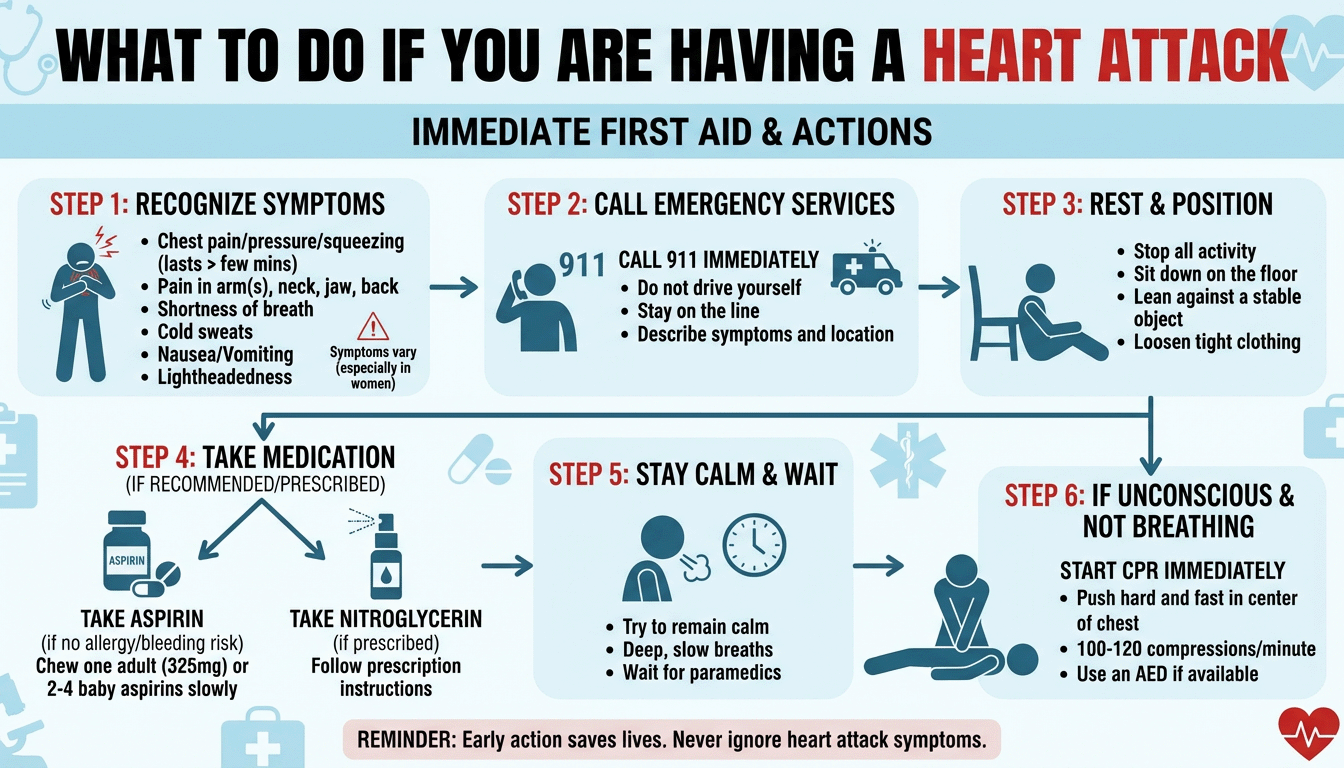
When Symptoms Signal a Medical Emergency
When heart attack warning signs show up, like new chest pain or shortness of breath, every minute counts. Quick, calm actions are key to a strong emergency response. They help protect the heart muscle.
Many people doubt the early signs or wait to see if they go away. Don’t wait. Check the key heart attack warning signs and act fast if you feel them.
Call 911 first: do not drive unless there’s no other option
Call 911 right away if you think you might be having a heart attack. Dispatchers can guide you, and paramedics start care immediately. This gets you to the right hospital faster and safer than driving yourself.
- If EMS is delayed, have someone else drive.
- Only drive yourself if there is no other option.
What to do while waiting: rest, nitroglycerin if prescribed
Sit or lie down to ease your heart’s work. Keep movements slow and steady. If a doctor has told you to take nitroglycerin, follow their instructions exactly. Don’t use someone else’s medicine.
- Loosen tight clothing and stay warm but not too hot.
- Watch your chest pain and breathing; note any changes for EMS.
Aspirin guidance: only if advised by clinicians or EMS
Aspirin can help, but it’s not always safe or timely. Please don’t wait to call 911 to take it. Only take aspirin if a doctor or EMS tells you to.
- Avoid aspirin if allergic, if told not to, or if bleeding risks are high.
- Follow local medical advice; EMS will tailor care to your needs.
Acting quickly at the first sign of heart attack warning signs—like sudden chest pain—is critical. It sets the stage for the best chance of emergency response and recovery.
How to Help Someone in Cardiac Arrest
A heart attack can cause sudden collapse. This happens when the heart stops due to an arrhythmia. Quick action with CPR and an AED can bring back a heartbeat. Anyone can help, and simple steps can make a big difference.
Stay calm, act fast, and get help on the way. A clear voice and steady hands guide others to assist while EMS is called.
Warning signs: sudden collapse, no normal breathing, no pulse
They may fall, become unresponsive, and not breathe normally. Gasping is not normal breathing. If there is no pulse or you are unsure, treat it as cardiac arrest and call 911 right away.
Ask someone to bring an AED. If alone with an adult, call first, then resume CPR. For quick guidance on actions, see this brief emergency treatment overview.
Hands-only CPR: 100–120 compressions per minute
Kneel beside the person. Place the heel of one hand in the center of the chest and the other on top. Lock your elbows and push hard and fast at 100–120 per minute, about 2 inches deep. Let the chest rise fully after each push.
Do not pause unless an AED is ready or the person begins breathing or moving. High-quality CPR keeps blood flowing during a heart attack emergency until EMS takes over.
Using an AED safely until EMS arrives
Turn on the AED and follow its voice prompts. Expose the chest, attach the pads as shown, and stand clear when the device analyzes the rhythm. If a shock is advised, make sure nobody is touching the person, then press the button.
Resume CPR right after any shock or “no shock” message. Keep alternating CPR and AED checks until professionals arrive. Widespread training in CPR and AED use helps communities respond faster to cardiac arrest and save more lives.
Angina Versus a Heart Attack: Knowing the Difference
Many wonder about the difference between angina and a heart attack. Both can cause chest pain. It’s essential to understand the signs early on.
Stable angina usually happens when you exert yourself, like climbing stairs. It feels like tightness or pressure. It gets better with rest or medicine.
Stable angina during exertion that improves with rest or medication
When you exert yourself, narrowed arteries can limit blood flow. This can cause a squeezing feeling. Resting and taking nitroglycerin can help relieve symptoms quickly.
- Occurs with exertion or stress
- Improves at rest within minutes
- Often responds to prescribed nitroglycerin
Persistent chest pain unrelieved by glyceryl trinitrate is a red flag
Chest pain that doesn’t improve with rest and medication is a warning sign. If nitroglycerin doesn’t work, try it again after five minutes. Pain that doesn’t go away, spreads, or comes with other symptoms might be a heart attack.
- Pain lasts more than a few minutes or keeps returning
- Spreads to the arm, back, neck, or jaw
- Comes with nausea, cold sweat, or dizziness
When to escalate and call emergency services
If symptoms are severe, new, or different from before, act fast. Call 911 if chest pain doesn’t go away with rest and medicine. Quick action is key when it’s hard to tell if it’s angina or a heart attack.
“If in doubt, treat it like an emergency. It is safer to be checked than to wait.”
Recurring pain that doesn’t get better with rest needs urgent care. Recognizing these signs can help prevent more damage from a heart attack.
Heart Attack Causes and Types
Heart attacks often start with damaged arteries and less blood to the heart. Knowing the causes and types helps people react quickly and ask the right questions at the hospital.
Most cases come from coronary artery disease, where atherosclerosis narrows the heart’s blood vessels. A cholesterol-rich plaque can rupture, leading to a clot. This blockage cuts off oxygen to the heart muscle.
Coronary artery disease and atherosclerosis
In coronary artery disease, plaque builds up inside a coronary artery. As atherosclerosis worsens, the artery becomes smaller. A crack in the plaque can cause a clot that blocks the artery, a serious cause of heart attacks.
High LDL, high blood pressure, and smoking speed up this process. Diabetes and chronic inflammation also harm the vessel lining and increase the risk—more Health articles.
STEMI versus NSTEMI and what ECG changes mean
Doctors classify myocardial infarction types by ECG patterns. A STEMI shows ST-segment elevation, indicating a sudden, complete blockage. An NSTEMI lacks this elevation and often means a partial blockage or intermittent flow.
Both types harm the heart muscle and need quick care. Blood tests for troponin and imaging, along with the ECG, help guide treatment.
Other causes: coronary spasm, SCAD, infections, including COVID-19
Not all heart attacks come from plaque rupture. A coronary spasm can suddenly block an artery, even in younger people or those with little plaque. Spontaneous coronary artery dissection (SCAD) tears the vessel wall and can block blood quickly.
Certain infections, like COVID-19, can inflame the heart or affect clotting. These causes add to the list of heart attack causes and types, beyond just atherosclerosis.
Heart Attack Risk Factors to Address
Knowing what causes heart attacks helps prevent them. It makes heart health a daily focus. This knowledge is key in the U.S., where heart attacks are common.
Small changes add up. Eating less salt and processed foods, moving more, and checking health numbers with a doctor can help. These actions build protection over time.
Age, tobacco use, high blood pressure, high LDL, and triglycerides
Heart attack risk goes up with age. Men over 45 and women over 55 are at higher risk. Smoking harms arteries, but quitting helps repair them quickly.
High blood pressure weakens artery walls, which is worse with high LDL or diabetes. High LDL and triglycerides narrow arteries, while HDL helps widen them.
For more on these causes and prevention steps, check out the Mayo Clinic. And keeping yourself safe from Pneumonia in this Network World News archive report.
Obesity, diabetes, metabolic syndrome, family history
Being overweight often means high blood pressure and high triglycerides. Diabetes damages blood vessels over time.
Metabolic syndrome, with signs like a big waist and high blood pressure, raises risk. A family history of early heart attacks means extra caution is needed.
Working on these risk factors is key to preventing heart attacks. It tackles common causes.
Inactive lifestyle, unhealthy diet, stress, and stimulant drug use
Sitting too much slows metabolism and raises blood pressure. Diets high in sugar and animal fats harm the heart.
Stress can trigger heart attacks. Cocaine and amphetamines can cause coronary spasm, making a risk into an emergency.
Regular exercise, healthy meals, and stress management help fight these risk factors.
History of preeclampsia and autoimmune conditions
Preeclampsia in pregnancy raises the lifetime risk, even years later, of autoimmune diseases like rheumatoid arthritis or lupus, which damage arteries.
Working with cardiology and rheumatology helps tailor prevention plans. This makes prevention realistic and practical.
Complications and Why Prompt Care Matters
Minutes matter when a heart attack strikes. Getting help fast saves heart muscle and lowers the risk of serious problems. Quick treatment helps prevent arrhythmias and cardiogenic shock, in which the heart can’t pump enough blood.
Some people get inflammation around the heart called pericarditis. Others face an immune response that leads to Dressler syndrome. Heart failure can also occur, damaging muscle and needing ongoing care.
Sudden cardiac arrest can happen without warning during or after a heart attack. Without quick CPR and defibrillation, it’s deadly. Calling 911 at the first sign of trouble is key to saving lives.
To learn more about signs, urgent steps, and treatments, see this CDC overview of heart attacks. Early EMS care, swift diagnosis, and treatment in accordance with guidelines are vital. They help avoid harm and speed recovery.
Signs of a Heart Attack Conclusion
A heart attack occurs when blood flow to the heart is blocked. A ruptured plaque and a clot often cause this blockage. Knowing the signs of a heart attack is key to changing the outcome.
Chest pressure or pain, discomfort spreading to the arm, back, neck, or jaw, and shortness of breath are essential signs. Cold sweat, nausea, lightheadedness, or indigestion-like pain also matter. Women may have milder symptoms, so they shouldn’t wait for severe chest pain to seek help.
If you see heart attack warning signs, call 911 right away. Rest while waiting for help to arrive. Use the prescribed nitroglycerin and follow your clinician’s or EMS’s advice on aspirin.
If someone collapses and is not breathing, start hands-only CPR. Do 100–120 compressions per minute. Use an AED as soon as it’s available. Quick action can protect the heart muscle and save lives.
Preventing heart attacks starts today. Tackle tobacco use, high blood pressure, unhealthy cholesterol, diabetes, and obesity. Move more, eat a heart-smart diet, manage stress, and avoid stimulant drugs.
People with a family history, preeclampsia, or autoimmune disease should work with their clinician to lower their risk. Small daily choices, along with regular checkups, can build a stronger heart.
Everyone can learn and share the warning signs of a heart attack. Spotting early clues and acting quickly helps both yourself and those you love. Prepared communities respond faster, recover better, and keep more lives on track.
Signs of a Heart Attack FAQ
What are the most important signs of a heart attack to recognize right away?
Heart attack warning signs include chest pain or pressure. This can feel like tightness, squeezing, or aching. It might spread to arms, shoulders, back, neck, jaw, teeth, or belly.
Shortness of breath, cold sweat, nausea, lightheadedness, or sudden dizziness are also common. Some people feel extreme fatigue or indigestion. Symptoms can vary, so if you suspect a heart attack, call 911 immediately.
What exactly is a heart attack, and why does every minute matter?
A heart attack happens when a coronary artery gets blocked. This blockage is usually caused by a cholesterol-rich plaque that ruptures. It starves the heart muscle of oxygen, leading to tissue death.
Rapid treatment is key to saving muscle, and calling 911 starts expert care sooner, improving survival chances.
How do blocked coronary arteries trigger a myocardial infarction?
Blocked arteries are often due to atherosclerosis, a buildup of fatty plaques. When a plaque ruptures, it can form a blood clot. This clot can block the artery, causing heart muscle damage.
Some heart attacks involve complete blockage (STEMI), while others are partial (NSTEMI).
How do plaque buildup, rupture, and clot formation lead to heart damage?
Over time, plaques narrow arteries and restrict blood flow. If a plaque ruptures, platelets stick to the site, forming a clot. This clot can suddenly block blood flow.
Without oxygen, heart cells begin to die within minutes. This can lead to arrhythmias, heart failure, or cardiogenic shock if not treated.
Why should someone call 911 instead of driving to the hospital?
Emergency services can start care en route, monitor heart rhythm, and administer oxygen if needed. They alert the hospital for rapid treatment. Driving delays care and can be dangerous if symptoms worsen.
In the U.S., call 911; in the U.K., call 999.
What does chest pain from a heart attack feel like?
People often describe pressure or tightness in the chest. It can feel like a belt tightening or a weight on the chest. The sensation can be steady or come and go, and it may be mild or severe.
Can heart attack pain spread beyond the chest?
Yes. Pain or discomfort can spread to arms, shoulders, back, neck, jaw, teeth, or upper belly. It may also feel like upper abdominal pressure or bad indigestion. Any unexplained radiating pain with chest pressure is a red flag.
What other heart attack symptoms should they watch for besides pain?
Shortness of breath, a cold sweat, lightheadedness or sudden dizziness, nausea or vomiting, unusual fatigue, and a sense of dread or anxiety can occur. Some people may cough or wheeze.
How do typical and atypical heart attack presentations differ?
Typical signs feature chest pressure plus radiating pain, shortness of breath, sweating, and nausea. Atypical symptoms can be subtle—indigestion, fatigue, back or jaw pain, or lightheadedness without chest pain. Atypical patterns are more common in women and older adults.
Can a heart attack feel like heartburn instead of crushing pain?
Yes. Heart attacks sometimes mimic heartburn or indigestion, with a burning feeling. If “indigestion” is new, severe, or paired with shortness of breath, sweat, or dizziness, treat it as a heart attack and call 911.
Do warning symptoms ever appear hours to weeks beforehand?
They can. Many people notice angina—chest pressure or discomfort with activity—that doesn’t go away with rest or recurs more often. Worsening or unrelieved angina can be an early warning sign. Escalating symptoms require urgent evaluation.
How might women’s heart attack symptoms look different?
Women may have brief or sharp neck, arm, or back pain; shortness of breath; unusual fatigue; indigestion; nausea; or jaw pain without classic chest pain. Because these signs are often dismissed, women should act quickly on any suspicious combination of symptoms.
What should someone do if a woman has these atypical symptoms?
The response is the same as for classic symptoms: call 911 immediately, have her rest, and follow the clinician’s instructions. If she has been prescribed nitroglycerin, use it as directed. Do not delay seeking care while deciding whether it’s “just indigestion.”
If symptoms suggest a heart attack, what is the first step?
Call 911 right away. Do not drive unless there is no other option. Emergency teams can begin treatment and speed arrival to a cardiac-ready hospital.
What should they do while waiting for EMS to arrive?
Have the person sit or lie down to reduce the heart’s workload. Loosen tight clothing. If nitroglycerin has been prescribed, take it exactly as directed. Keep the phone nearby and unlock the door for responders.
Should they take aspirin during a suspected heart attack?
Aspirin can reduce clotting, but it’s not for everyone. Do not delay calling 911 to take it. Only take aspirin if advised by a clinician or EMS, considering bleeding risks or medication interactions.
What are the warning signs of sudden cardiac arrest during a heart attack?
Sudden collapse, unresponsiveness, no normal breathing, and no pulse. This is a life-threatening emergency. Call 911 immediately.
How do they perform hands-only CPR?
If the person isn’t breathing normally and no pulse is found, begin hands-only CPR. Push hard and fast in the center of the chest at 100–120 compressions per minute, about 2 inches deep, allowing full recoil. Continue until EMS arrives or an AED is ready.
How can an AED be used safely by bystanders?
Please turn it on and follow the voice prompts. Expose the chest, attach pads as shown, and stand clear during analysis and shock delivery. Resume compressions immediately after a shock or when instructed. AEDs are designed for safe public use.
How is angina different from a heart attack?
Angina is chest pain from temporarily reduced blood flow, often brought on by exertion and relieved by rest or prescribed nitroglycerin. A heart attack involves prolonged blockage with heart muscle damage. Angina that changes, lasts longer, or occurs at rest needs urgent care.
When does chest pain unrelieved by glyceryl trinitrate signal a heart attack?
If angina does not improve within about 5 minutes after nitroglycerin, recurs quickly, or is accompanied by shortness of breath, dizziness, or feeling unwell, call 911 immediately. Persistent pain is a red flag.
When should someone escalate from self-care to emergency services?
At the first sign of heart attack symptoms—chest pressure, radiating pain, shortness of breath, cold sweat, nausea, or lightheadedness—call 911. Do not wait to see if it passes.
What causes most heart attacks?
Most result from coronary artery disease, where atherosclerotic plaques narrow the coronary arteries. When a plaque ruptures, a clot can fully or partially block blood flow, triggering a myocardial infarction.
What is the difference between STEMI and NSTEMI?
A STEMI usually reflects a complete acute occlusion and shows ST-segment elevation on an ECG, requiring urgent reperfusion therapy. An NSTEMI often involves partial blockage with no ST elevation but causes heart damage and needs prompt treatment.
Are there other heart attack causes besides plaque rupture?
Yes. Coronary artery spasm (Prinzmetal’s), spontaneous coronary artery dissection (SCAD), and infections, including COVID-19, can injure the heart and lead to infarction or myocarditis-related damage.
What are the key heart attack risk factors people can address?
Major heart attack risk factors include age (men 45+, women 55+), tobacco use and secondhand smoke, high blood pressure, high LDL and triglycerides, low HDL, diabetes, obesity, and metabolic syndrome. A family history of an early heart attack also raises risk.
How do lifestyle and medical conditions influence heart attack risk?
An inactive lifestyle, an unhealthy diet high in sugar, trans fats, processed foods, and salt, and high stress increase the risk. Stimulant drug use, such as cocaine or amphetamines, can trigger spasms and heart attacks. A history of preeclampsia and autoimmune diseases like rheumatoid arthritis or lupus raises long-term risk.
What complications can follow a heart attack?
Possible complications include dangerous arrhythmias, cardiogenic shock, heart failure, pericarditis (including Dressler syndrome), and sudden cardiac arrest. Prompt recognition and treatment limit heart muscle loss and lower the chance of these outcomes.
How can someone help prevent a heart attack?
Prevention starts with quitting smoking, controlling blood pressure, cholesterol, and blood sugar, staying active, maintaining a healthy weight, eating a heart-healthy diet, managing stress, and following medical advice. Regular checkups help detect and manage risk factors early.
What should they remember if symptoms start suddenly?
Act fast. Call 911 at the first sign of heart attack symptoms—chest pressure, radiating pain, shortness of breath, cold sweat, nausea, or lightheadedness. Rest, use nitroglycerin if prescribed, and follow emergency guidance. Quick action saves lives.









